Müllerian Anomalies and Fertility
Müllerian anomalies, congenital malformations of the female reproductive tract, arise from abnormal development of the Müllerian ducts during embryogenesis. These anomalies affect approximately 5–6% of women overall but are more prevalent in those with infertility (8–10%) or recurrent pregnancy loss (12–25%). Their impact on fertility and pregnancy outcomes varies widely, making early diagnosis and tailored management critical.
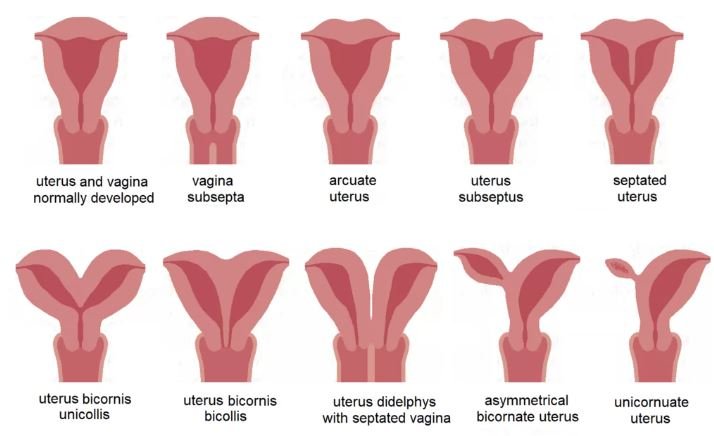
Types of Müllerian Anomalies
The 2021 ASRM classification categorizes these anomalies into distinct groups, emphasizing uterine, cervical, and vaginal variations:
Agenesis/Hypoplasia (e.g., Mayer-Rokitansky-Küster-Hauser syndrome/MRKH): Absence of the uterus and upper vagina, requiring surrogacy for biological children.
Lateral Fusion Defects:
Septate uterus (most common): A fibrous or muscular septum divides the uterine cavity, linked to recurrent miscarriage due to poor blood supply.
Bicornuate uterus: A heart-shaped uterus with a partial indentation; associated with preterm birth and cervical incompetence.
Uterus didelphys: Two separate uterine bodies and cervixes, often with vaginal septa.
Vertical Fusion Defects: Transverse vaginal septum or cervical agenesis, causing menstrual obstruction.
Unicornuate uterus: A single "banana-shaped" uterine horn, often paired with a rudimentary horn and renal anomalies (40% of cases).
Impact on Fertility
Müllerian anomalies can disrupt conception, implantation, and pregnancy maintenance:
MRKH Syndrome: Prevents natural pregnancy, though ovarian function remains intact (surrogacy required).
Septate Uterus: Highest risk of recurrent miscarriage (up to 60% loss rate) due to avascular septal tissue. Surgical resection improves live birth rates to 83%.
Unicornuate Uterus: Smaller cavity and reduced blood flow increase miscarriage (25–38%) and preterm delivery (40–50%) risks.
Bicornuate/Didelphys Uterus: Higher rates of preterm labor (39–56%) and fetal malpresentation (34–37%).
Key Stat: Women with Müllerian anomalies have a 3.5x higher risk of preterm birth and 8.8x higher risk of malpresentation compared to those with normal anatomy.
Diagnosis
Accurate diagnosis relies on imaging and clinical evaluation:
3D Transvaginal Ultrasound: First-line for assessing uterine contour and cavity structure.
MRI: Gold standard for complex cases, offering detailed visualization of uterine and renal anatomy.
Hysterosalpingography (HSG): Evaluates tubal patency but lacks detail on external uterine shape.
Hysteroscopy/Laparoscopy: Direct visualization for surgical planning, especially for septate or obstructed anomalies.
Treatment Strategies
Management depends on anomaly type, symptoms, and reproductive goals:
Surgical Corrections:
Septum Resection: Hysteroscopic metroplasty for septate uterus improves live birth rates from <10% to >80%.
Vaginal Septum Excision: Relieves obstruction and improves menstrual flow.
Strassman Metroplasty: For bicornuate uterus, though evidence on efficacy is mixed.
Assisted Reproductive Technologies (ART):
IVF is recommended for concurrent tubal or male factor infertility.
Surrogacy for MRKH or cervical agenesis.
Preconception Care:
Renal imaging (30% have associated anomalies) and genetic counseling 13.
Lifestyle optimization and management of comorbidities like PCOS or endometriosis 6.
Pregnancy Management
Close monitoring is essential due to heightened risks:
Preterm Birth Prevention: Cervical length screening and progesterone supplementation, though efficacy varies.
Malpresentation: Cesarean delivery is common (34–47% of cases).
Placental Complications: Higher rates of abruption, previa, and retained placenta necessitate expert care.
Case Example: A woman with unicornuate uterus achieved term delivery after aggressive monitoring, cerclage, and preterm labor management.
Conclusion
Müllerian anomalies pose unique challenges, but advances in imaging, surgery, and ART offer hope. Key steps include:
Early diagnosis via 3D ultrasound or MRI.
Individualized treatment (e.g., septum resection for recurrent loss).
Multidisciplinary care involving MFM specialists, reproductive endocrinologists, and surgeons.
For patients, understanding their specific anomaly and engaging in preconception planning can significantly enhance reproductive outcomes.
Explore in more depth: ASRM guidelines.
Disclaimer: This blog post is for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider for personalized recommendations.